The web Browser you are currently using is unsupported, and some features of this site may not work as intended. Please update to a modern browser such as Chrome, Firefox or Edge to experience all features Michigan.gov has to offer.
Safe Sleep
Safe Sleep
Below are the American Academy of Pediatrics Recommendations for a Safe Sleeping Environment.
Follow these recommendations to create a safe sleep environment for your baby, but while you read through them keep these things in mind:
- These steps aren't always as simple as they sound. If you need help or feel overwhelmed, talk with your healthcare provider to create a plan that is best for you and your baby. Reach out to family and friends to ask for help.
- County services through the Michigan Department of Health and Human Services often provide safe sleep resources. The resources available may include complimentary safety products, sleep sacks, or play yards, as well as educational materials and classes. Check out this list to see what your county has to offer.
- It is also important that you and your baby stay healthy - by obtaining regular prenatal care, taking baby to wellness checkups and obtaining recommended immunizations.
Share this information with all family, friends, and childcare providers who may care for your baby to ensure they follow the safe sleep steps.
"Building Blocks of Safe Sleep" (Safe Sleep) a video by the Michigan Department of Health and Human Services.
When you build safe sleep into your baby's sleep routine, you can keep them safer. Learn the building blocks of infant safe sleep at Michigan.gov/SafeSleep.
Safe Sleep Recommendations:
-
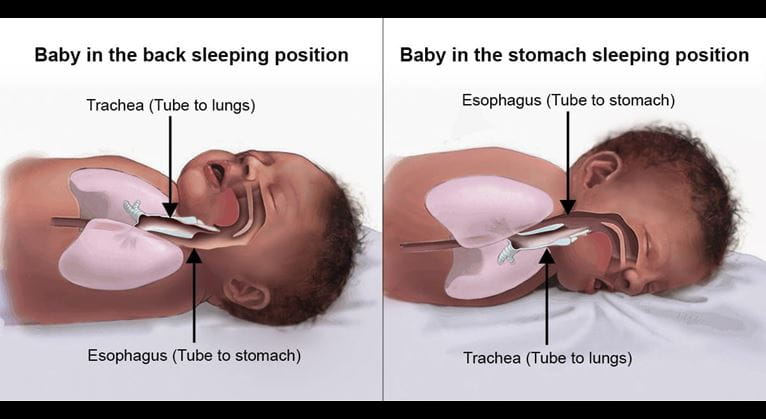
1. Always place your baby on their back to sleep.
Back sleeping protects a baby's airway and ensures access to fresh air. Once your baby can roll from back to stomach and from stomach to back, he or she can be allowed to remain in the sleep position that they choose.
The risks associated with putting a baby to sleep on their stomach include:
- Babies on the stomach can sleep too deeply and may not wake up to take a breath.
- Babies, especially when young, can have poor head and neck control and may not physically be able to move to take a breath if needed.
-
2. Babies should sleep on an approved sleep surface like a crib, bassinet, or pack 'n play, with a firm mattress and tight fitted sheet.
There are risks associated with unsafe sleep surfaces and practices.
- Babies sleeping with an adult or another child in a bed can get stuck or wedged between a standard bed and the wall, furniture or other objects.
- Babies are not safe sleeping on couches or chairs. They can suffocate on or get wedged between the cushions.
In an emergency, an alternative device with a firm, flat, non-inclined surface (e.g., box, basket, or dresser drawer) with thin, firm padding may be used temporarily. However, this alternative device should be replaced as soon as a Consumer Product Safety Commission-approved surface is available.
-
3. Babies should sleep alone. Understand the increased risk of sharing sleep spaces.
Sharing sleep spaces increases the risk of infant mortality.
The risk is increased by more than 10 times the baseline risk of parent–infant bed sharing when:
- Bed sharing with someone who is impaired in their alertness or ability to arouse because of fatigue or use of sedating medications (e.g., certain antidepressants, pain medications) or substances (e.g., alcohol, illicit drugs).
- Bed sharing with a current smoker (even if the smoker does not smoke in bed) or if the pregnant parent smoked during pregnancy.
- Bed sharing on a soft surface, such as a waterbed, old mattress, sofa, couch, or armchair.
The risk is increased by 5–10 times the baseline risk of parent–infant bed sharing when:
- A baby born at full-term and normal weight is less than 4 months old, even if neither parent smokes, even if the infant is breastfed.
- This is a particularly vulnerable time, so parents who choose to feed their infants less than 4 months old in bed need to be especially vigilant to avoid falling asleep.
- Bed sharing with anyone who is not the infant’s parent, including nonparental caregivers and other children.
The risk is increased by 2–5 times the baseline risk of parent–infant bed sharing when:
- Preterm or low birth weight infant, even if neither parent smokes.
- Bed sharing with soft bedding accessories, such as pillows or blankets.
-
4. No pillows, blankets, comforters, stuffed animals or other objects should be in your baby's sleep area.
- Also keep other soft objects away from an infants sleep space like quilts, comforters, mattress toppers, fur-like materials and loose bedding like nonfitted sheets.
- These objects increase the risk of SIDS, suffocation, entrapment, and strangulation.
-
5. Your baby should sleep where you can see and hear them.
- Share your room, not your bed.
- For the first six months, infants should sleep on a separate sleep surface where parents can see and hear them.
-
6. Avoid covering your baby's head when sleeping or overheating your baby.
MDHHS has shared the following information about preventing overheating in sleeping babies:
- After hospital discharge, your baby should not wear a hat when sleeping.
- If you think your baby is cold, dress him or her in a footed sleeper with a sleep sack right for his or her size and age.
Signs a baby is good for sleep:
- Ears are the same color as their body
- Hands and feet are cool to the touch
- Nothing is covering their head
- Back of the neck and chest feel warm but not hot
- They're dressed right for the room, wearing a light sleeper or onesie under their sleep sack
- Their sleep sack material is appropriate for the weather and the room temperature
-
7. Sleep surfaces should have an incline of less than 10 degrees.
- Sleep surfaces with inclines of >10 degrees are unsafe for infant sleep.
- Swings, bouncy seats, and car seats could lead to a baby having difficulty breathing or have head or neck injuries.
- If your baby falls asleep in a swing, bouncy seat, car seat, or other sitting devices, he or she should be moved to a crib, bassinet, or pack 'n play as soon as it is possible.
-
8. Additional Recommendations:
- Feeding of human milk is recommended because it is associated with a reduced risk of SIDS.
- Participate in supervised, awake tummy time daily.
- Avoid smoke and nicotine exposure during pregnancy and after birth.
- Avoid alcohol, marijuana, opioids, and illicit drug use during pregnancy and after birth.
- Consider offering your baby a pacifier at naptime and bedtime.
- Do not use home cardiorespiratory monitors as a strategy to reduce the risk of SIDS.
-
Frequently Asked Questions about Safe Sleep Recommendations
The MDHHS has additional information about Safe Sleep including a list of FAQs. Click here to access their resources.
Information for fire departments & EMS agencies to be certified in safe sleep.
Every enrollee gets a custom welcome email and the full support of the EMS for Children Program as well as MDHHS Infant Safe Sleep and local safe sleep resources. Each department is able to customize their training and resource plans. Using this link departments can:
- Find program materials
- Enroll in the program
- Complete the attestation form once all required steps are completed to let MDHHS know they want to certify
Want to learn more about keeping your infant safe?
MSU Extension has partnered with the Livingston County Child Abuse Prevention Council to create a self-directed online infant safety course called “Sleeping, Crying, Driving.” This three-part course contains videos and interactive content on infant safe sleep, how to handle extended infant crying and guidelines for transporting your child safely. Click here for Registration Information.
Additional Resources
There are lots of resources and tools available to learn more about safe sleep recommendations and guidelines. Below are links to some of those resources.
